 A new test that, by simultaneously studying 115 genetic hereditary mutations, will map the genetic risk is offered for a year to all the patients with ovarian cancer at the European Institute of Oncology (EIO). This is the program for the launch of the laboratory of Clinical Genomics of the EIO. The program has been presented by Roberto Orecchia, Scientific Director, Pier Giuseppe Pelicci, Director of Research, Nicoletta Colombo, Director of the Gynecology Program, Bernardo Bonanni, Director of Preventive and Oncological Genetics, Massimo Barberis, Director of Histopathological and Molecular Diagnostics Unit.
A new test that, by simultaneously studying 115 genetic hereditary mutations, will map the genetic risk is offered for a year to all the patients with ovarian cancer at the European Institute of Oncology (EIO). This is the program for the launch of the laboratory of Clinical Genomics of the EIO. The program has been presented by Roberto Orecchia, Scientific Director, Pier Giuseppe Pelicci, Director of Research, Nicoletta Colombo, Director of the Gynecology Program, Bernardo Bonanni, Director of Preventive and Oncological Genetics, Massimo Barberis, Director of Histopathological and Molecular Diagnostics Unit.
“The activity of Clinical Genomics lead us in line with the world movement of Precision Medicine, launched in USA in 2015 by the ex-president Obama with the ‘Precision Medicine Initiative’, and is the flagship of EIO research –states Orecchia-. We are living an extraordinary moment. In 2016, our Impact Factor (an index basically measuring the prestige of scientific research) is 3.165, with a huge step ahead of about 300 points compared to last year; our publication records reached a peak of 450, with 50 more papers published compared to 2015. In 2016, we started 104 new clinical studies and conducted 524 studies that were already active. In total, in 2016, 4017 patients asked to be part of experimental protocols in EIO”.
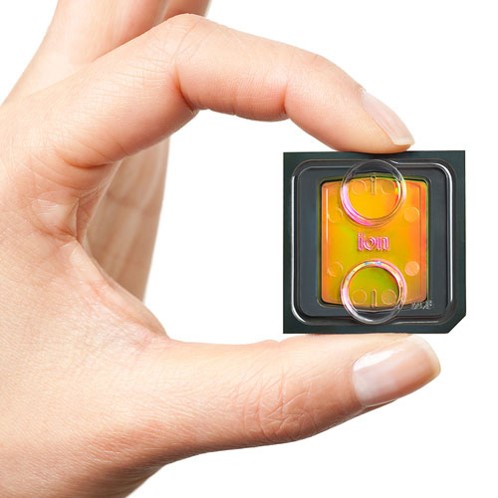
“The EIO genomics project has a main goal: creating ‘a genetic passport’ per each patient, a microchip -or Oncochip- containing all the molecular data related to tumors- explains Dr Pelicci. A computerized document carrying the required information to set up prevention (for patients too, in case of familiarity risk), diagnosis and targeted therapies. Our first step goes towards prevention. Using forefront technology (Next Generation Sequencing) we set up a rapid, precise and economically sustainable genetic test capable of mapping hereditary genetic risk, analyzing in a single chip 115 known genetic mutations. Main advantages are: first, the ability to better identify each person risk and start personalized protection protocols; second, identifying a higher number of potentially hereditary tumors and, thus, extending protection to a higher number of people, particularly to families; third, knowing more genetic mutations will allow us to produce more preventive targeted drugs, possibly hindering cancer incidence. In the near future, besides hereditary risk, we might have information on the individual risk, unraveling from the study of the DNA whether our cells have been negatively affected by the environment. Shortly, each of us will have a complete map of its own risk to get cancer”.
“The new generation tests, using multigene panels capable of analyzing several genes at the same time, are an unbelievable resource for prevention –says Dr Bonanni-. It is very important to access a targeted genetic test even after evaluation of personal and familiar history, but in some cases, the result might be negative because the genes involved may be different from those analyzed. The new possibility of having information on a more ample range of genes potentially carrying hereditary mutations opens the door to a more complete and personalized ‘medicine of high risk’, which means the possibility to establish protective protocols for the individual and familiar risk to get disease, through more effective clinical programs going from special imaging control to dietary recommendations, from pharmacological therapy to prophylactic surgery.”
“In some cases molecular alterations, including hereditary mutations, present in tumors are not necessarily present in non-tumor cells –says Dr Barberis-. For this reason, in EIO we integrate genetics data with molecular pathology data. The goal is to extend this approach to each patient. In many cases, by studying sick cells we can find genetic alterations targetable by new drugs able to provide concrete benefit. Ovarian cancer is a typical case”.
“For ovarian cancer –concludes Dr Colombo- knowing if the patient’s genome has hereditary mutations, particularly in BRAC1 and BRCA2 genes, is crucial for prevention as well as for the treatment. Patients carrying BRCA mutations have, indeed, a high probability to respond to therapy with drugs named PARP inhibitors, in addition to being “good responders” to traditional chemotherapy. Therefore, identifying this mutation means finding a targeted treatment. Moreover, knowing that BRCA mutation is hereditary, we are authorized to propose the test to other family members too, in order to protect them from an eventual augmented risk in case they are positive. For this reason, we decided to offer for a year the complete genetic test to all EIO patients with ovarian cancer. This will be the first initiative of clinical research of the Women’s Cancer Center, the newborn multidisciplinary centre for women care. This is a unique initiative in Italy that we believe can contribute to halt ovarian cancer incidence, a difficult disease that today is still the first cause of mortality for gynecological neoplasia”.